FACTS vs. FICTION
Epilepsy is NOT a form of mental illness.
It is a well-documented neurological condition that affects the brain’s electrical activity.
People with epilepsy are NOT less intelligent than those without epilepsy.
While some with epilepsy may have cognitive impairments, these are more often related to the underlying cause of their epilepsy (such as a brain injury) rather than epilepsy itself.
Mental Health challenges CANNOT cause epilepsy.
Epilepsy is a physical disorder that has a neurological basis. While emotional stress can trigger seizures in some people, it is not the underlying cause of epilepsy.
WHAT IS STIGMA?
Stigma is a negative label or judgment that people put on others who are different from them in some way, like their race, gender, sexual orientation, or health condition. This can make the person feel ashamed, isolated, or discriminated against and can prevent them from being treated fairly or getting the help they need.
Children with epilepsy are particularly vulnerable to experiencing stigma, so much so, in fact, that parents may even withhold the medical diagnosis from school personnel for fear of the stigma their child may face.
Discrimination and Epilepsy
Enacted stigma – which may also be referred to as discrimination – refers to the actual behaviors or actions that people take towards those who are stigmatized, such as:
- Exclusion
- Teasing/harassing
- Bullying
- or even Violence
Felt Stigma and Epilepsy
Felt stigma – sometimes referred to as internalized or self-stigma – refers to the negative beliefs, feelings, and attitudes that individuals who belong to a stigmatized group may have about themselves as a result of societal stereotypes and discrimination.
For example, a child with epilepsy may internalize negative messages about the condition and begin to feel ashamed or embarrassed about it. This can lead to a child feeling:
- Lonely or isolated
- Powerless
- Shame or embarrassment
Social Consequences of Epilepsy
Children with epilepsy often experience both enacted stigma and felt stigma. This can have social consequences such as:
- Difficulty making new friends – in part due to lower self-esteem and reduced confidence in social situations
- Social exclusion – due to fear or misunderstandings of seizures by their peers or adults or fears of getting hurt
- Difficulty with transitions – due to concerns about disclosure and stigma, moving or starting a new school can be especially difficult
Personal Impacts of Epilepsy
It will be no surprise that in addition to the social impacts of stigma, there may be significant personal impacts that a child experiences as a result of stigma, including:
- Feeling of powerlessness
- Insecurity
- Self-isolation
- Dependence on others – even when they ‘should be’ more independent
- Shame
- Feelings of being ‘less than’ or inferior
DEPRESSION AND ANXIETY
Depression and anxiety are two of the more significant personal impacts often experienced by children with epilepsy.

Anxiety
- Anxiety in children with epilepsy often arises in response to the unpredictability and lack of control associated with seizures. Children may overestimate the threat posed by future seizures or underestimate their ability to cope with the seizures.
Did you know?
- One study found that up to 40% of children with epilepsy develop anxiety disorders compared to just under 9% of children without epilepsy.
- Other studies have found the prevalence of anxiety disorders may even be as high as 50% of children with epilepsy.
- Anticipatory anxiety may include worrying about the threat of having a seizure.
- Social phobias may develop for fear of having a seizure in public and being embarrassed.
Depression
- Depression is frequently under-recognized and under-treated in children who have epilepsy.
Did you know?
- Up to 30% of children and adolescents who have been diagnosed with seizures also have depression

Children with anxiety may:
- Appear more clingy than usual
- Be restless or fidgety
- Complain of stomachaches
- Express negative thoughts or generalized worrying
- Display changes in eating or sleeping habits
- Have bouts of unexplained crying
- Experience acute, overwhelming panic attacks
- Get upset or angry more quickly
- Display obsessive-compulsive tendencies
Here are a few things we all can do to help a child who’s struggling:
- Provide a safe and supportive environment by promoting a culture of acceptance.
- Encourage open communication without fear of judgment.
- Identify those at risk by learning to recognize symptoms.
- Provide referrals to school mental health services or mental health professionals.
- Offer accommodations and flexibility as needed.
- Educate parents and guardians on the signs and symptoms of depression.
- Normalize seeking help for mental health concerns.
- Foster a positive school culture that promotes inclusion, kindness, and empathy.
- Establish peer support programs through the school or in partnership with local organizations.
- Promote self-care such as exercise, meditation, or other coping strategies.
BULLYING
You can learn more about Epilepsy and Bullying and how you can best support children with epilepsy in this presentation from our Back to School webinar which was held in August 2023.
And when the concern is especially serious:
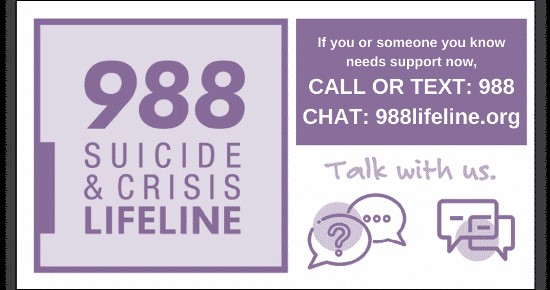
A recent report noted that as many as 20% of children and teens with epilepsy experience suicidal thoughts at some point in their life. Such statistics are frightening to all of us.
Here are a few suggestions should you have particular concerns about a student hurting themself:
- Don’t wait. Get help from other people or agencies that specialize in crisis intervention and suicide prevention – including the 9-8-8 Suicide and Crisis Lifeline (Dial 988).
- Act. Remove the method, such as any weapons or pills.
- Get involved and be available. Show interest and support.
- Be direct. Talk openly and matter-of-factly about suicide.
- Really listen and allow them to express their feelings.

INABILITY TO CONTROL SEIZURES
Decreased ability to control seizures can also contribute to mental health challenges. In addition to seizure-related stressors, there may be other influences on a person’s mental health.
Medications
Anti-epileptic drug therapy (AEDs) are used to control seizures. AEDs can cause side effects such as:
- Disruption in sleep patterns.
- Drowsiness, fatigue, dizziness, and nausea.
- Cognitive slowing, difficulties with memory, paying attention, or concentrating.
- Mood changes, including an increased risk of suicidal thoughts.
Sleep Deprivation
Epilepsy often causes sleep deprivation; sleep deprivation can trigger seizures.
- Frequent seizures while sleeping can cause anxiety about going to sleep-disrupting sleep even further.
- Poor sleep can lead to hyperactivity and/or inattention, depression, or anxiety.
- Lack of sleep makes a person more irritable, short-tempered, and less able to handle stress.
Stress
Stress increases the risk of mental health challenges in people with epilepsy.
- Stress in early childhood can disrupt the development and limbic structures of the brain – which are responsible for mood regulation and emotion.
- Stress can affect sleep by:
- Making it difficult to fall asleep.
- Altering the sleep structure.
- Leading to poor quality sleep.
- Increasing frequency and intensity of nightmares.
Learn More
This information about Mental Health and Epilepsy is part of the OnDemand Seizure First Aid and Recognition Training for School Personnel available 24/7 on our website.
Acknowledgements
The development of the Mental Health and Epilepsy module of our OnDemand Seizure First Aid and Recognition Training for School Personnel was made possible through funding provided by Jazz Pharmaceuticals.

All content was created by an ad hoc committee of Epilepsy Alliance America member organizations in partnership with the Continuing Learning Education Program at Rutgers University School of Public Health and reviewed by members of Epilepsy Alliance America’s National Professional Advisory Committee.
Updated September 13, 2023
